Painkiller warning as household pills found to supercharge antibiotic resistance - with elderly most at risk

The over-the-counter remedies are inadvertently contributing to one of medicine's most pressing challenges, scientists have warned
Don't Miss
Most Read
Scientists have uncovered alarming evidence that widely used painkillers ibuprofen and paracetamol are fuelling antibiotic resistance.
The groundbreaking research, conducted by the University of South Australia, demonstrates how these household medications trigger increased bacterial mutations in E. coli, a common pathogen responsible for gut and urinary tract infections.
This marks the first investigation of its kind examining how non-antibiotic drugs interact with bacterial resistance mechanisms.
The study's findings reveal that both medications significantly enhance E. coli's ability to develop resistance when exposed to antibiotics.
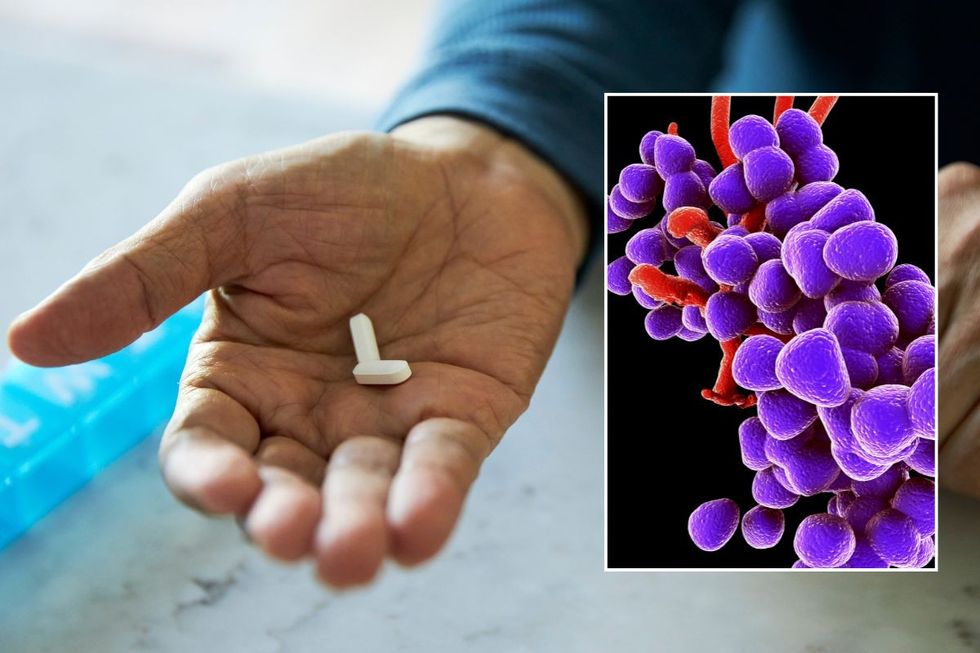
Antimicrobial resistance directly caused 1.27 million deaths worldwide in 2019
|GETTY
The discovery carries profound implications for global health, particularly given that antimicrobial resistance directly caused 1.27 million deaths worldwide in 2019, according to World Health Organization data.
The research examined how ibuprofen and paracetamol interact with ciprofloxacin, a broad-spectrum antibiotic commonly prescribed for skin, gut and urinary tract infections.
When E. coli bacteria encountered the antibiotic alongside these painkillers, they developed significantly more genetic mutations compared to antibiotic exposure alone.
The combination effect proved particularly concerning, with bacteria not only becoming highly resistant to ciprofloxacin but also showing increased resistance to multiple other antibiotics from different classes.
The study revealed that both medications activate bacterial defence systems designed to expel antibiotics, rendering the treatments less effective.
This amplification effect, when the drugs are used together, represents a previously unknown mechanism by which common household medications can undermine antibiotic therapy, potentially compromising treatment outcomes for routine infections.
The implications prove especially serious for residential aged care facilities, where elderly residents routinely receive multiple medications simultaneously.
These environments create ideal breeding grounds for antibiotic-resistant bacteria to flourish, as older patients typically require various treatments for pain management, sleep disorders, and blood pressure control alongside potential antibiotic therapy.
Associate Professor Rietie Venter, who led the research, broke down the particular vulnerability of this population.
She explained: "This is especially prevalent in residential aged care facilities, where older people are more likely to be prescribed multiple medications, not just antibiotics, but also drugs for pain, sleep, or blood pressure, making it an ideal breeding ground for gut bacteria to become resistant to antibiotics."
The study examined nine medications commonly administered in aged care settings, highlighting the complex medication interactions occurring in these facilities daily.
The research team advocates for heightened awareness regarding medication interactions, particularly among patients receiving long-term treatment regimens.
LATEST DEVELOPMENTS

Older people in care facilities are more likely to be prescribed multiple medications
|PEXELS
Associate Professor Venter stressed that antibiotic resistance has evolved beyond traditional concerns about antibiotic misuse alone.
She said: "Antibiotic resistance isn't just about antibiotics anymore. This study is a clear reminder that we need to carefully consider the risks of using multiple medications, particularly in aged care, where residents are often prescribed a mix of long-term treatments."
The researchers noted that discontinuing these essential medications is not the solution.
Instead, they call for comprehensive studies examining drug interactions across all patient populations receiving extended medication courses, enabling healthcare providers to better understand how common pharmaceuticals may compromise antibiotic effectiveness beyond simple two-drug combinations.